What is toxoplasmosis?
 Toxoplasmosis is a disease caused by a single-celled parasite called Toxoplasma gondii (T. gondii). Toxoplasmosis is one of the most common parasitic diseases and has been found in nearly all warm-blooded animals, including pets and humans. Despite the high prevalence of T. gondii infection, the parasite rarely causes significant clinical disease in cats-or any species.
Toxoplasmosis is a disease caused by a single-celled parasite called Toxoplasma gondii (T. gondii). Toxoplasmosis is one of the most common parasitic diseases and has been found in nearly all warm-blooded animals, including pets and humans. Despite the high prevalence of T. gondii infection, the parasite rarely causes significant clinical disease in cats-or any species.
What causes toxoplasmosis?
The life cycle of Toxoplasma gondii is complex and involves two types of host-definitive and intermediate. Cats, both wild and domestic, are the only definitive hosts for Toxoplasma gondii. This means that the parasite can only produce oocysts (eggs) when infecting a cat. When a cat ingests an infected prey (or other infected raw meat) the parasite is released into the cat’s digestive tract. The organisms then multiply in the wall of the small intestine and produce oocysts during what is known as the intraintestinal infection cycle. These oocysts are then excreted in great numbers in the cat’s feces. Cats previously unexposed to T. gondii will usually begin shedding oocysts between three and 10 days after ingestion of infected tissue, and continue shedding for around 10 to 14 days, during which time many millions of oocysts may be produced. Oocysts are very resistant and may survive in the environment for well over a year.
During the intraintestinal infection cycle in the cat, some T. gondii organisms released from the ingested cysts penetrate more deeply into the wall of the intestine and multiply as tachyzoite forms. These forms then spread out from the intestine to other parts of the cat’s body, starting the extraintestinal infection cycle. Eventually, the cat’s immune system restrains this stage of the organism, which then enters a dormant or “resting” stage by forming cysts in muscles and brain. These cysts contain bradyzoites, or slowly multiplying organisms.
Other animals, including humans, are intermediate hosts of Toxoplasma gondii. These hosts can become infected but do not produce oocysts. Oocysts passed in a cat’s feces are not immediately infectious to other animals. They must first go through a process called sporulation, which takes one to five days depending on environmental conditions. Once sporulated, oocysts are infectious to cats, people, and other intermediate hosts. Intermediate hosts become infected through ingestion of sporulated oocysts, and this infection results in formation of tissue cysts in various tissues of the body. Tissue cysts remain in the intermediate host for life and are infectious to cats, people and other intermediate hosts if the cyst-containing tissue is eaten.
How will toxoplasmosis affect my cat?
Most cats infected with T. gondii will not show any symptoms. Occasionally, however, clinical disease-toxoplasmosis-occurs. When disease does occur, it may develop when the cat’s immune response is not adequate to stop the spread of tachyzoite forms. The disease is more likely to occur in cats with suppressed immune systems, including young kittens and cats with feline leukemia virus (FELV) or feline immunodeficiency virus (FIV).
The most common symptoms of toxoplasmosis include fever, loss of appetite, and lethargy. Other symptoms may occur depending on whether the infection is acute or chronic, and where the parasite is found in the body. In the lungs, T. gondii infection can lead to pneumonia, which will cause respiratory distress of gradually increasing severity. Toxoplasmosis can also affect the eyes and central nervous system, producing inflammation of the retina or anterior ocular chamber, abnormal pupil size and responsiveness to light, blindness, incoordination, heightened sensitivity to touch, personality changes, circling, head pressing, twitching of the ears, difficulty in chewing and swallowing food, seizures, and loss of control over urination and defecation.
How is toxoplasmosis diagnosed in cats?
Toxoplasmosis is usually diagnosed based on the history, signs of illness, and the results of supportive laboratory tests. Measurement of IgG and IgM antibodies to Toxoplasma gondii in the blood can help diagnose toxoplasmosis. The presence of significant IgG antibodies to T. gondii in a healthy cat suggests that the cat has been previously infected and now is most likely immune and not excreting oocysts. The presence of significant IgM antibodies to T. gondii, however, suggests an active infection of the cat. The absence of T. gondii antibodies of both types in a healthy cat suggests that the cat is susceptible to infection and thus would shed oocysts for one to two weeks following infection.
Sometimes the oocysts can be found in the feces, but this is not a reliable method of diagnosis because they look similar to some other parasites. Also, cats shed the oocysts for only a short period of time and often are not shedding the oocysts when they are showing signs of disease. A definitive diagnosis requires microscopic examination of tissues or tissue impression smears for distinctive pathologic changes and the presence of tachyzoites.
Can toxoplasmosis be treated?
Most cats that have toxoplasmosis can recover with treatment. Treatment usually involves a course of an antibiotic called Clindamycin. Other drugs that are used include pyrimethamine and sulfadiazine, which act together to inhibit T. gondii reproduction. Treatment must be started as soon as possible after diagnosis and continued for several days after signs have disappeared. In acute illness, treatment is sometimes started on the basis of a high antibody titer in the first test. If clinical improvement is not seen within two to three days, the diagnosis of toxoplasmosis should be questioned.
No vaccine is as yet available to prevent either T. gondii infection or toxoplasmosis in cats, humans, or other species.
Can I “catch” toxoplasmosis from my cat?
Because cats only shed the organism for a few days in their entire life, the chance of human exposure is small. Owning a cat does not mean you will be infected with the disease. It is unlikely that you would be exposed to the parasite by touching an infected cat, because cats usually do not carry the parasite on their fur. It is also unlikely that you can become infected through cat bites or scratches. In addition, cats kept indoors that do not hunt prey or are not fed raw meat are not likely to be infected with T. gondii.
In the United States, people are much more likely to become infected through eating raw meat and unwashed fruits and vegetables than from handling cat feces.
How are people infected with Toxoplasma gondii?
Contact with oocyst-contaminated soil is probably the major means by which many different species-rodents, ground-feeding birds, sheep, goats, pigs, and cattle, as well as humans living in developing countries-are exposed to Toxoplasma gondii. In the industrialized nations, most transmission to humans is probably due to eating undercooked infected meat, particularly lamb and pork. People also become infected by eating unwashed fruits and vegetables. The organism can sometimes be present in some unpasteurized dairy products, such as goat’s milk. Toxoplasma gondii can also be transmitted directly from pregnant woman to unborn child when the mother becomes infected during pregnancy.
There are two populations at high risk for infection with Toxoplasma gondii; pregnant women and immunodeficient individuals. Congenital infection is of greatest concern in humans. About one-third to one-half of human infants born to mothers who have acquired Toxoplasma during that pregnancy are infected. The vast majority of women infected during pregnancy have no symptoms of the infection themselves. The majority of infected infants will show no symptoms of toxoplasmosis at birth, but many are likely to develop signs of infection later in life. Loss of vision, mental retardation, loss of hearing, and death in severe cases, are the symptoms of toxoplasmosis in congenitally infected children.
In immunodeficient people-those undergoing immunosuppressive therapy (e.g., for cancer or organ transplantation) or those with an immunosuppressive disease such as AIDS-enlargement of the lymph nodes, ocular and central nervous-system disturbances, respiratory disease, and heart disease are among the more characteristic symptoms. In these patients-especially those with AIDS-relapses of the disease are common, and the mortality rate is high. In the past, immunodeficient people and pregnant women were advised to avoid cats. However, the Centers for Disease Control (CDC) now advises that this is not necessary.
What can I do to prevent toxoplasmosis?
There are several general sanitation and food safety steps you can take to reduce your chances of becoming infected with Toxoplasma:
- Do not eat raw or undercooked meat. Meat should be cooked to a temperature of at least 160°F for 20 minutes.
- Do not drink unpasteurized milk.
- Do not eat unwashed fruits and vegetables.
- Wash hands and food preparation surfaces with warm soapy water after handling raw meat.
- Wear gloves when gardening. Wash hands after gardening.
- Wash hands before eating (especially for children).
- Keep children’s sandboxes covered.
- Do not drink water from the environment unless it is boiled.
- Do not feed raw meat or undercooked meat to cats. Also, do not give them unpasteurized milk.
- Do not allow cats to hunt or roam.
- Do not allow cats to use a garden or children’s play area as their litter box.
- Remove feces from the litter box daily and clean with boiling or scalding water.
- Pregnant women, and persons with suppressed immune systems, should not clean the litter box.
- Control rodent populations and other potential intermediate hosts.
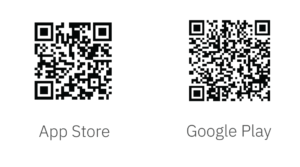
If you think you or your pet has been exposed to toxoplasmosis, or are showing any symptoms, please contact your doctor, or your veterinarian for your pet.
Some info courtesy of the American Association of Feline Practitioners and the Cornell Feline Health Center, Cornell University, College of Veterinary Medicine, Ithaca, NY 14853-6401.